When you or someone you know is diagnosed with ovarian cancer, your health care team will provide a type and stage when sharing the news. Knowing your type and stage of ovarian cancer will help you to understand the recommended treatment options and allow you to take a more active role in decision-making alongside your care team.
Types of ovarian cancer
There are several types of ovarian cancers. These types are broken out by the types of cells they originated from, how they appear to researchers when being studied, and how they behave. Ovarian cancer starts from three common cell types:
- Epithelial cells – epithelial cells cover the outer lining of the ovaries. Most ovarian cancers are epithelial cell tumors.
- Germ cells – germ cells produce the eggs (ova) and some tumors can form in these cells
- Sex cord stromal cells – these cells are tissue cells that provide structure to the ovary to hold it together and some ovarian tumors can form in this tissue. These cells produce hormones like estrogens and androgens (other sex hormones).
1. Epithelial ovarian tumors
Epithelial cell tumors develop from the cells covering the outer surface of the ovary. These tumors can be benign (not cancer), borderline (low cancer potential), or malignant (cancer).
There are several other types of benign (not cancer) and borderline (low potential for cancer) epithelial tumors including:
Benign:
- serous cystadenomas
- mucinous cystadenomas
- Brenner tumors
Borderline:
Under the microscope, some ovarian epithelial tumors do not clearly identify as cancerous. These are called borderline tumors or tumors of low malignant potential (LMP tumors).
- serous borderline neoplasm
- mucinous borderline neoplasm
- endometrioid borderline neoplasms
Epithelial ovarian cancer grows in the tissue that lines the ovaries. This is the most common type of ovarian cancer, accounting for 85 to 90 percent of all cancers of the ovaries. Unfortunately, about 80 percent of women diagnosed with epithelial ovarian cancer are not diagnosed until the disease is advanced in stage.
Types of epithelial ovarian cancer:
- serous carcinomas (most common) – 70-80%
- endometrioid carcinoma (less common) – 10%
- clear cell carcinoma (less common) – 10%
- mucinous carcinoma (less common) – 3%
Epithelial ovarian cancer: Serous Type
Serous ovarian cancers are the most common type of epithelial cell ovarian cancers and can include both high and low-grade cancers.
- High-grade serous ovarian cancer is the most common type of epithelial ovarian cancer. These tumor cells look very abnormal and are fast-growing. It is now thought that most high-grade serous ovarian cancers start in cells at the far end of the fallopian tube, rather than the surface of the ovary. These early cancer cells then spread to the ovary and grow.
- Low-grade serous ovarian cancer is a much less common type of epithelial ovarian cancer. It looks the most like normal cells and is slow-growing. It typically affects younger ages between 40 and 60 but can affect women of all ages, accounting for about 2-5% of epithelial ovarian cancers. It is often more advanced at the time of diagnosis and does not respond well to chemotherapy. Because of this, initial treatment usually requires debulking surgery (surgery to remove as much visible tumor as possible). These tumors will almost always recur.
Epithelial ovarian cancer: Endometrioid Type
Endometrioid cell ovarian cancer accounts for about 10% of all epithelial ovarian cancers. It is usually diagnosed in younger women and at an early stage. These tumors are often associated with endometriosis and Lynch syndrome. It is also sometimes seen also with endometrial cancer.
A note about endometriosis and ovarian cancer: the overall lifetime risk of developing ovarian cancer due to having endometriosis is relatively low. If you are concerned about how endometriosis might affect your risk, talk to your doctor.
Epithelial ovarian cancer: Clear Cell Type
Clear cell ovarian cancer accounts for 5-10% of all epithelial ovarian cancers and is seen more often in people who have had endometriosis. Like other forms of ovarian cancer, it is usually treated with surgery and chemotherapy, although clear cell carcinoma is also very resistant to chemotherapy.
Epithelial ovarian cancer: Mucinous Type
Mucinous cell ovarian cancer is the rarest form and accounts for about 3% of all epithelial ovarian cancers. In most cases, it is localized and has a good prognosis.
Other cancers similar to epithelial ovarian cancer:
There are other cancers that are similar to epithelial ovarian cancer. These include:
- primary peritoneal carcinoma
- fallopian tube cancer
Primary peritoneal carcinoma (PPC) is rare. It looks very similar to epithelial ovarian cancer that has spread to the abdomen. This type of cancer forms in the peritoneum (the tissue that lines the abdominal wall and covers organs). The cells of the peritoneal lining develop from the same type of cell that lines the surface of the ovary and fallopian tube. PPC can sometimes spread to the ovaries. It is a close relative of epithelial ovarian cancer. Symptoms and treatment are similar to that of ovarian cancer.
Fallopian tube cancer is also rare and is similar to epithelial ovarian cancer. It begins in the fallopian tube, the tube that carries an egg from the ovary to the uterus.
For more information about PPC and Fallopian tube cancers, visit the American Cancer Society and Foundation for Women’s Cancer.
2. Germ cell ovarian tumors
Germ cell tumors develop from the cells that produce the ova or eggs. Most germ cell tumors are benign (non-cancerous), although some are cancerous and may be life-threatening. Germ cell tumors account for less than 2% of ovarian cancers and typically have a good outlook. There are several subtypes of germ cell cancers including:
- Immature teratomas
- dysgerminomas
- endodermal sinus tumors (yolk sac tumor)
- Choriocarinomas
- Embryonal carcinoma
Teratomas can be benign (not cancer) and it is known as a mature teratoma. It is the most common form of benign germ cell tumor. It is often called a dermoid cyst because its makeup is similar to skin (dermis). Surgery is usually done to remove the teratoma.
Dysgerminomas are the most common ovarian germ cell cancers but are rare. It is usually found in younger women in their teens and twenties. They are usually diagnosed at an early stage and most are surgically removed successfully.
For more information about these types of germ cell ovarian tumors, visit the American Cancer Society.
3. Sex Cord Stromal ovarian tumors
Stromal cell tumors account for about less than 5% of ovarian cancers, are usually found at early stage and have a good outlook. They develop from the connective tissue cells that hold the ovary together and produce hormones (estrogens and androgens). There are several types of stromal cell cancers including:
- Granulosa cell tumor
- Sertoli cell tumor
- Sertoli-Leydig cell tumor
There are several types of benign sex cord stromal tumors including:
- Thecoma
- Fibroma
- Fibrothecoma
For more information about these types of stromal cell ovarian tumors, visit the American Cancer Society.
Other rare ovarian cancers
Small-cell ovarian cancer is a very rare, aggressive type of cancer that has two subtypes – hypercalcemic type and pulmonary type. The hypercalcemic type is diagnosed more often in young women in their teens and twenties and is more resistant to chemotherapy. The pulmonary type is diagnosed in older women and is more sensitive to chemotherapy.
Ovarian cysts
Ovarian cysts are fluid-filled sacs found inside the ovary and are very common. In fact, they can form as a normal part of the ovulation process. They usually go away on their own without any treatment. Ovarian cysts can become a problem, particularly in women who are not ovulating, such as those after menopause. In this case, a doctor should do more testing. Especially if it does not go away.
Most cysts are benign (not cancer), but a small number of cysts can be malignant (cancer). The risk for ovarian cancer increases with age. Postmenopausal women with cysts have a higher risk for ovarian cancer. Be sure to talk to your doctor about your risk. The only way to know for sure is to surgically remove it. Cysts can be imaged and those that look to be benign can be observed for a time or removed with surgery.
Ovarian cysts may not cause any symptoms or can be quite painful. The pain may be dull or sharp and may come and go. Cysts can rupture which can cause severe and sudden pain. Rarely can they cause an emergency, but if you experience pain, fever, vomiting, dizziness, weakness or rapid breathing, seek medical attention.
Questions to ask your doctor about ovarian cysts:
- What is causing my symptoms? If a cyst, what might be causing it?
- What tests might I need?
- Will my cyst go away on its own, or will I need treatment?
- What type of cyst do I have and what should I know about my risk for ovarian cancer?
- Do you have printed materials or brochures I can have? What websites do you recommend?
For more detailed information about ovarian cysts, visit the Office on Women’s Health and additional information found here.
Stages of ovarian cancer
When ovarian cancer is diagnosed, doctors will try to determine if the cancer has spread, and if so, how far. This process is called staging. The cancer type and stage can be determined during surgery. The stage of the cancer tells us how advanced the cancer is and now to treat it.
There are two staging systems used. They are very similar but the FIGO (Federation of Gynecology and Obstetrics) is used most. In the FIGO system, ovarian cancer stage is defined by 3 main areas of growth:
- The extent of the primary tumor
- The spread of cancer to nearby lymph nodes
- The spread of cancer to distant sites in the body (other organs).
Ovarian cancer stages are numbered 1 to 4. You will often see these stages written as stage I, II, III or IV. These four stages are further broken down into smaller groups which describe the extent of the cancer in more detail. Determining the stage of your cancer is essential because it will help your healthcare provider determine the best treatment plan for you.
Staging ovarian cancer
Stage I ovarian cancer
Stage II ovarian cancer
Stage III ovarian cancer
Stage IV ovarian cancer
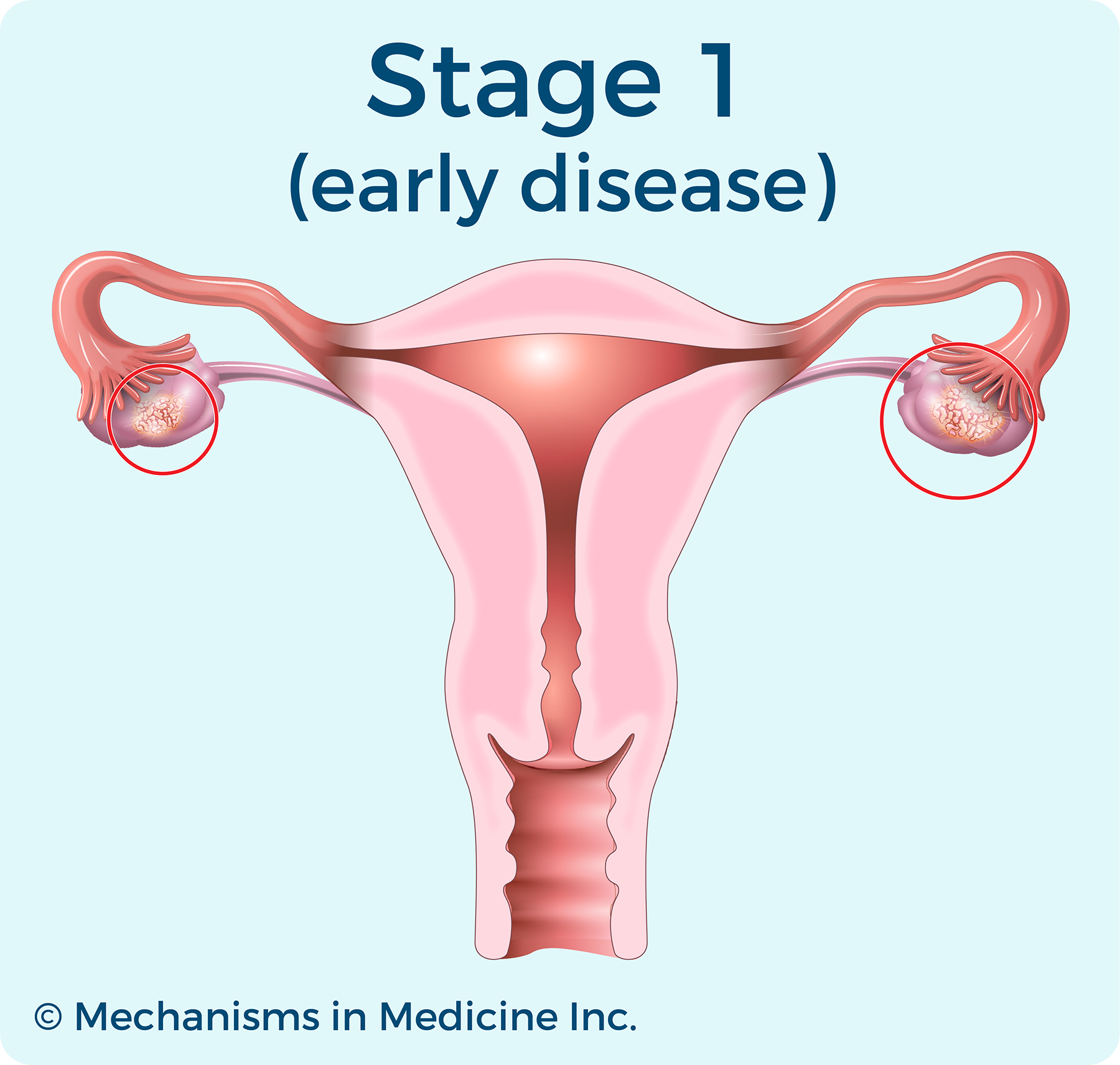
Stage I ovarian cancer
In Stage I, cancer is in one or both ovaries and may also be on the outer surface of the ovaries or in fluids in the abdomen. It is divided into three substages – A, B, and C:
- Stage 1A – Cancer is in one ovary, or fallopian tube. There is no cancer on the outside surface of the ovary. No cancer cells are found in ascites or washings.
- Stage 1B – Cancer is in both ovaries or fallopian tubes. The capsules are intact and there is no cancer on the outside surface of the ovaries. No cancer cells are found in ascites or washings.
- Stage 1C – Cancer is in one or both ovaries and one or more of the following has also happened:
- Stage 1C1 – The tumor ruptures while it is being removed surgically, called intraoperative surgical spill.
- Stage 1C2 – The tumor wall is ruptured before surgery, or there is cancer on the surface of the ovary or fallopian tube.
- Stage 1C3 – Cancer cells are found in fluid buildup in the abdominal cavity, called ascites, or in the samples of fluid from the peritoneal cavity taken during surgery.
Stage II ovarian cancer
In Stage II, cancer has spread to the fallopian tubes or other organs in the pelvis. It is divided into two substages – A and B:
- Stage 2A – The cancer has spread to the uterus and/or fallopian tubes and/or the ovaries.
- Stage 2B- The cancer has spread to other tissues within the pelvis. This may include the bladder, colon, rectum, or the peritoneum within the pelvis. The peritoneum is the tissue that lines the inside of the abdomen and pelvis and covers most organs in this space.
Stage III ovarian cancer
Stage III
In Stage III, cancer has spread to the lymph nodes; to other places in the abdomen such as the lining, or peritoneum; or to the outer surface of the spleen or liver. It is divided into three substages – A, B, and C:
- Stage 3A1 – Cancer has spread outside the pelvis, but only to lymph nodes in the back of the abdomen— called retroperitoneal lymph nodes.
- Stage 3A2 – Cancer has spread to the tissue lining the abdomen. The cancer is so small it can only be seen with a microscope. There may also be cancer in lymph nodes in the back of the abdomen.
Stage IV ovarian cancer
Stage IV
Stage IV, cancer has spread to lymph nodes outside the abdomen or to inside the lungs, spleen, liver, or brain. There are two substages, A and B:
- Stage 4A – There are cancer cells in the fluid around the lungs. This is called a malignant pleural effusion.
- Stage 4B – Cancer has spread to the inside of the liver or spleen, to distant lymph nodes, or to other organs outside the abdomen.
For more information: You and Ovarian Cancer: An Animated Patient’s Guide to Ovarian Cancer
Tumor grade
Doctor’s also describe ovarian cancer by its grade. A tumor’s grade is different from the cancer stage, as it describes how healthy the cancer cells look when viewed under a microscope. The cancer grade is a rating of how fast the cancer is expected to grow and spread. The cancer’s grade may help predict how quickly the cancer will spread. It also helps determine a treatment plan decision.
Grading ovarian cancer
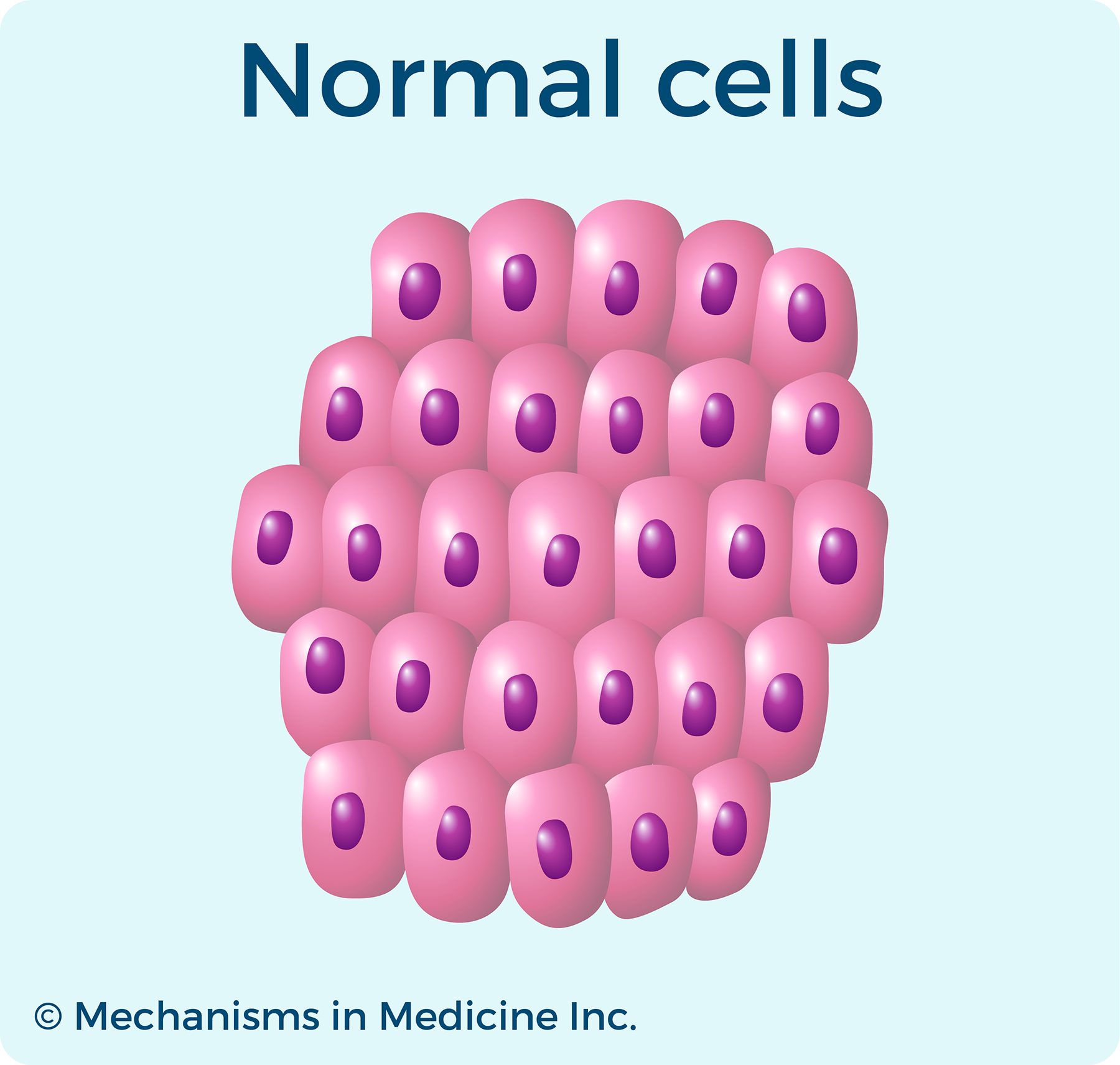
Normal cells
Low grade ovarian cancer
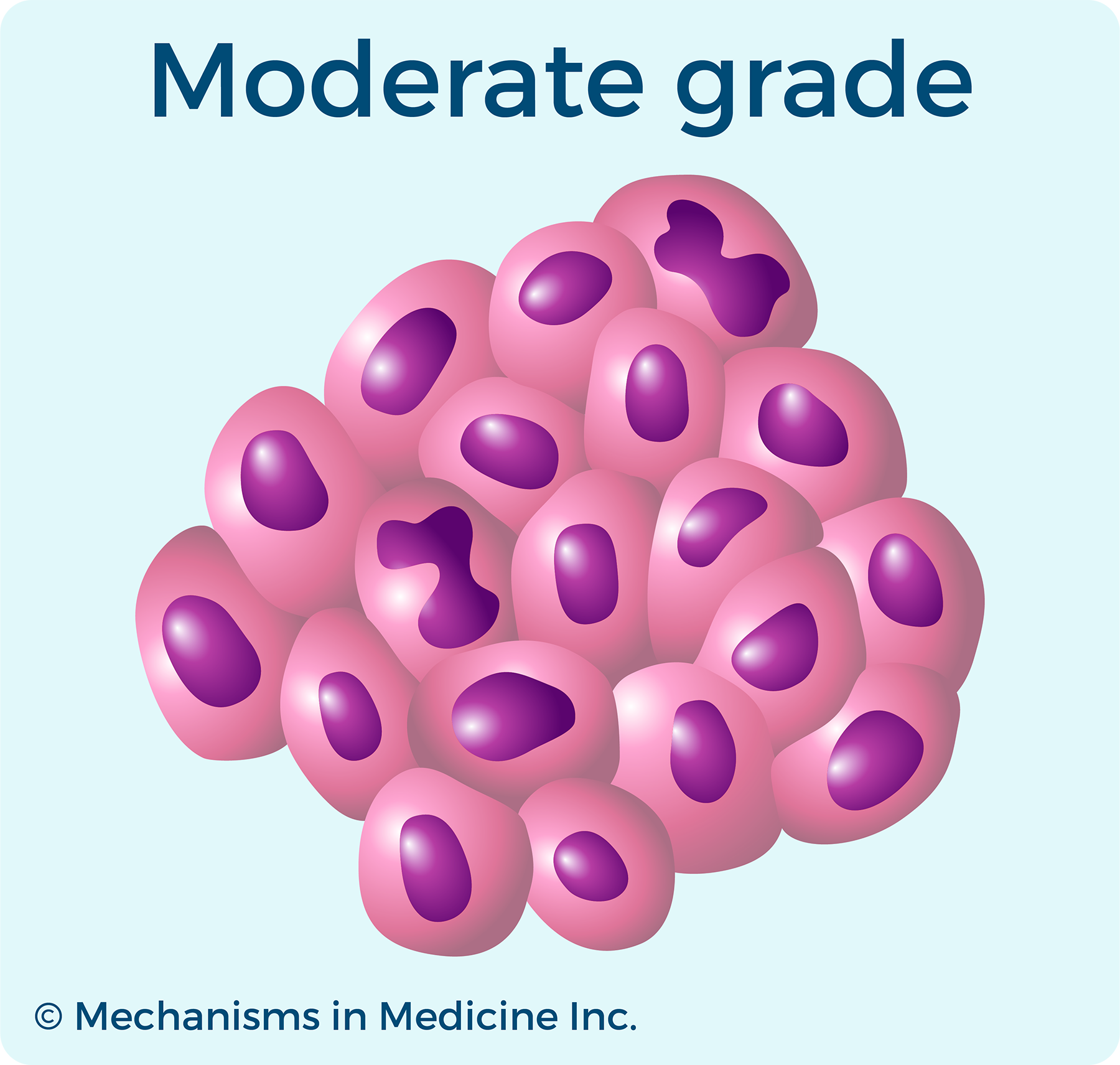
Moderate grade ovarian cancer
High grade ovarian cancer
Grades of ovarian cancer
Grade 1 describes cancer tissue that contains many healthy-looking cells, which is referred to as “well-differentiated” tissue.
Grade 2 describes cancer tissue in which more cells appear abnormal than healthy, also called “moderately differentiated.”
Grade 3 describes cancer tissue with a lack of normal structure in which more abnormal than healthy cells appear, also called “poorly differentiated” or “undifferentiated.”
For more information: You and Ovarian Cancer: An Animated Patient’s Guide to Ovarian Cancer
Useful Resources

Questions to Ask Your Doctor - Newly Diagnosed
Have you been newly diagnosed with ovarian cancer? Download these questions to ask your doctor.
Questions to Ask Your Doctor - Low-Grade Serous Ovarian Cancer
Do you have low-grade serous ovarian cancer? Download these questions to ask your doctor.
References:
- What Is Ovarian Cancer | Ovarian Tumors and Cysts
- Primary Peritoneal – Foundation for Women’s Cancer
- Ovarian Cysts – Diagnosis and Treatment – Mayo Clinic. 6 Aug. 2022
- Green, Andrew E., MD. Ovarian Cancer: Practice Essentials, Background, Pathophysiology. 17 Nov. 2022
- Grisham, Rachel N., MD. “Low-Grade Serous Carcinoma of the Ovary.” Cancer Network, 4 Jan. 2022
- Levitan, Dave. “Endometrioid Ovarian Cancer Presents Earlier, Offers Better Survival Than Serous Carcinoma.” Cancer Network, 4 Jan. 2022
- Epithelial Ovarian Cancer | Cancer Research UK
- Primary Peritoneal – Foundation for Women’s Cancer
- “Guidelines for Patients Details.” NCCN
- Chen S, Li Y, Qian L, Deng S, Liu L, Xiao W and Zhou Y (2021) A Review of the Clinical Characteristics and Novel Molecular Subtypes of Endometrioid Ovarian Cancer. Front. Oncol. 11:668151. doi: 10.3389/fonc.2021.668151
- Morice, Philippe, et al. “Mucinous Ovarian Carcinoma.” New England Journal of Medicine, edited by Dan L. Longo, vol. 380, no. 13, Massachusetts Medical Society, Mar. 2019, pp. 1256–66. https://doi.org/10.1056/nejmra1813254
- Agarwal S, Pandey P, Ralli M, Singh S. Ovarian Small Cell Carcinoma: A Rare Case Report and Review of Literature. Iran J Pathol. 2018 Winter;13(1):99-102. PMID: 29731803; PMCID: PMC5929396
Page Last Reviewed January 2023